LGBTQ Sex Myths, Preconceptions, and Safety Tips
LGBTQ Sex Myths, Preconceptions, and Safety Tips
by LaShay Harvey, M.Ed.
Thinking about the time your child will become sexually active, now or years from now, can be scary for any parent. And if your child identifies as LGBTQ, this time can be particularly challenging with so many myths and concerns circulating. Parents of LGBTQ teens often express concern about their teen’s sexual safety. So here is a shortlist of myths, preconceived notions, and safer sex tips about “gay sex” to help you and your teen better navigate their sexuality.
Myths & Preconceptions
All teens are promiscuous. By 15, about 16% of teens have had sex. By 17, that number has more than doubled. This statistic is not meant to frighten you but rather to highlight what may or may not happen for most teens. The truth is that most youth are anxious about sex because of the mixed messages they receive every day (e.g. boys should have sex with everyone, while girls should have sex with NO ONE!). Most youth who have ever had sex have only had one partner, and they have usually had oral sex before they ever have intercourse. In addition to the sexual values you and your family have worked to instill, it is important to know that teens are navigating their sexuality and behavior choices with whatever amount of knowledge they have.
My teen isn’t thinking about/having sex. It’s true that some teens are, in fact, asexual: a person who rarely, if ever, experiences sexual attraction for another person. However, many teenagers are entering romantic and/or sexual relationships and are experiencing feelings of attraction and arousal. All of these experiences are “normal.” So no matter where your child is on the spectrum, they will most likely at least have thoughts about sex.
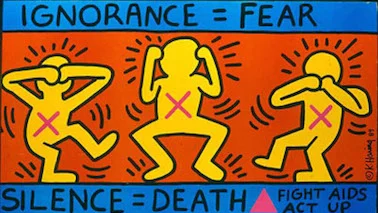
STIs are high with teens. It is true that teenagers have higher rates of sexually transmitted infections than adults do. However, context is very important to understanding this phenomenon. Teens often have high rates of STIs because they do not have the correct information about sex or access to safer sex protection, not because they are having sex with a lot of people.
This is a phase. Sexual orientation is often fluid for young people. Adolescence is a time characterized by intense changes for young people, and their sexual attractions are not spared. So your child’s sexual orientation or gender identity might be a phase, but it might not be. Whether or not they are the same person 10 years from now is not always the most important aspect to focus on. But making sure they are sexually and emotionally healthy years from now is. By talking honestly and safely with young people now about their sexuality and providing them with the tools that will be necessary to enter ANY relationship, they will be successful AND healthy for many years to come!
Safe(r) Sex
Protection. If your child is LGBTQ, there are plenty of safe and safer sex tools young people can use to keep themselves safe, if they decide to have sex. There are condoms that can be used by all genders and orientations. There are condoms made of latex that are traditionally worn on the penis and others made of polyurethane that can be worn inside the vagina.
There are also other barrier methods of protection. For female or lesbian-identified youth who have sex with other female-identified or lesbian youth, there are dental dams that cover the genitals and allow for safer sex. All of these condoms and dental dams are safe to use, very effective at preventing sexually transmitted infections (STI) when used correctly, and inexpensive. Actually, many health departments and school health clinics will have these condoms on hand so that youth can access them and receive accurate information on how to use them.
Testing. One of the best ways young people (and everyone, for that matter!) can protect themselves and their sexual partners is by knowing their STI and HIV status. One of the most mature decisions a young person (or anyone, for that matter!) can make about their sexual health is deciding when and where to get tested for STIs and HIV. Encouraging your LGBTQ teenager to know their status is a major step in the direction of their sexual health. It is important to note that just because your teen decides to get tested for STIs or HIV does not necessarily mean they think they are positive. It actually suggests that a young person is taking proactive steps to being a sexually healthy individual. And isn’t that what we want—sexually healthy teens?
Communication. Teens are wonderfully complex. They can be inappropriate, obnoxious, and utterly confusing at times. Yet they can also be exceptionally smart and critical, understanding, and fun. In spite of the ups and downs and back and forth, LGBTQ teens have feelings about many things, and they have myriad ways of expressing those feelings. If young people can feel safe discussing and expressing their feelings about sexuality, no matter how complex and confusing, with a parent or guardian, they will be more likely to feel safe discussing and expressing their feelings with a sexual partner. If the only people that your teenager can talk about sex to are their peers, they may not be getting the most helpful, safe, or accurate information. Consider giving your teen room to practice their sexual communication skills with you or someone you trust.
Pleasure. There is quite a bit of research that links pleasure during an LGBTQ teen’s first sexual experience with their future sexual risk-taking. In short, if sex is pleasurable for LGBTQ teens, they are more likely to practice safer sex. If teens are engaged in discussion on pleasure and safer sex practices (condoms, communication, testing, etc.), they will be more likely to exercise those practices. However, the messages most LGBTQ teens receive about the sex they can and will have are often very negative. But you can change that!
LaShay Harvey, M.Ed., is a sexologist, professor, and researcher from the south, currently living in Baltimore, MD. LaShay teaches a course on sexuality and a course on gender at The University of Baltimore. She also coordinates a study on pelvic inflammatory disease (PID) at The Johns Hopkins University.
Want to become a volunteer writer? Tell us here!







Talking to your child about safer sex practices can always be a tough conversation to have, but especially if you have to have the conversation as your child is coming into an LGBTQ identity at the same time. Ellen Kate has five tips to help you through it.